Raising the bar with air quality through multi-stage filtration and energy-efficient HVAC systems that are responsive and adaptive, constitute an innovative way towards a modern and sustainable hospital environment, writes Dr Iyad Al-Attar, independent air filtration consultant
The earlier purpose of most hospitals was to house – not cure – the sick in tightly packed rows of beds in dark open wards. Then, in the early 1900s, hospitals started focusing on curing patients and using X-rays and cardiographs, which revolutionised patient care and saved the lives of millions. However, keeping the machines needed for treatment near patients represented a significant challenge for the staff and fundamentally changed how designers approached hospital layouts.
Today, staying overnight in a hospital could mean experiencing a shared room poorly lit by flickering fluorescent lamps and with no windows. Furthermore, the persistent odour might keep the patient up all night, if the cacophony of beeping from various old machines does not. Likewise, research has established that Hospital Acquired Infections (HAIs), cross-contamination and Sick Building Syndrome, owing to fluctuating temperatures and poor Indoor Air Quality, can worsen the health condition of patients[1-3]. So today, raising the bar of air quality through multi-stage filtration and energy-efficient HVAC systems that are responsive and adaptive, constitute an innovative way towards a modern and sustainable hospital environment.

Dr Iyad Al-Attar
Additional studies have suggested that balancing natural and artificial lighting through windows and lamps, respectively, can impact the healing process of patients[4,5]. However, avoiding temperature fluctuations from external sources, through exterior windows, is critical to the indoor environment. Therefore, the appropriateness of HVAC system selection and performance is paramount to controlling the climate, in terms of temperature and moisture. Climate control does not necessarily mean the thermal comfort relevant to human occupants; in a hospital context, it addresses the appropriate temperature and humidity for wounds, so that chemicals and enzymatic processes are optimally engaged in the healing process with the metabolism of cells and tissue[6]. Furthermore, despite efforts to attain the best air quality, the contaminants carried indoors from outdoors represent a risk for infection outbreak, even after the treated patient has left the hospital[7-9].
Perceived and conceived hospital design
Hospitals require more than just a design facelift; therefore, the narrative alters how hospitals are perceived and conceived. Hospitals do not have to be daunting, especially since patients are usually not in the best emotional state, and feel vulnerable due to their health conditions. While a modern and sustainable hospital environment should provide the best medical expertise and a pleasant place for occupants, it is equally important to have such a healing space free of contamination. HVAC and filtration systems can play a greater role in improving air quality while meeting thermal comfort targets. Ultimately, patient satisfaction is attainable if better air quality, filtration systems and operational efficiency are integrated towards sustainable performance.
The evolving nature of hospital design
Healthcare facilities are continually evolving to help revolutionise and redefine how care be delivered in the future. Architects incorporate the planting of trees to bring a calming ambience to hospital facilities, as shown in Figure 1. Architects also consider other parameters to optimise their designs, such as the building’s geographical location, the site’s topography, annual weather and aerosol data. Furthermore, humanity can realise its dream of a utopian hospital that embraces sustainability by generating its power with a minimal environmental footprint and using its waste as a resource.
The visiting pollutants
In a hospital environment, the methods of reducing contaminant concentrations range from source control to dilution with ventilation and extraction with filtration. The dispersion of various pollutants humans can carry indoors is a significant challenge to the IAQ rendered by filtration-intensive systems. When patients talk, sneeze and cough, they produce many particles light enough to remain suspended in the air and spread infection[10]. In addition, poor visitors’ health conditions can impact the air quality in the hospital environment and the wellbeing of the staff to work and patients to heal and recover[11]. Our respiratory systems are often exposed to multiple pollutants simultaneously. Consequently, it may be difficult to correlate specific symptoms to a given pollutant when they co-exist in solid or in gaseous state, or as bioaerosols.
Innovative hospital design must leverage various advanced technologies, not only those relevant to air filtration and HVAC systems. That would enable the hospital environment to engage its facilities to make real-time adjustments to facilitate a sterile therapeutic environment. Ultimately, realising that no engineering measure can single-handedly enhance air quality sustainably is critical to the need for such performance integration. Overlooking the role of ventilation, entertaining modest maintenance plans, and weak approaches to air quality improvements will hinder any plans to exit the status quo and may result in additional pandemics[13-15]. The solution cannot simply lie in frequent filter replacement to resolve air quality issues. That can easily fall under the sustainability knife, which endorses the circularity concept of extending the lifetime of air filters in operation balanced by sustainable performance. Therefore, further research on sustainable air filters and HVAC systems performance is required to reduce the transmission of airborne contaminants.
Operating theatres in focus
The challenge of managing the hospital built environment lies in engineering and interfacing several parameters in complex building settings. Indoors, healthcare facility design is more complex than other building types, influencing HVAC, air quality and filtration requirements. For example, HVAC requirements for the design of operating rooms range from regulating temperature and moisture to appropriate space pressurisation between adjacent zones. In addition, operating theatres require clean room applications, mandating advanced air filtration systems to yield acceptable air quality. And laminar air diffusion represents the final critical step towards achieving thermal comfort by utilising equal clean air distribution in individual zones.
Air filter performance
The final stage of filter performance is their disposal after usage. Leaving behind loaded filters, such as HEPA types, at the storage of regular waste disposal cannot be a sustainable way forward (Figure 2). These filters collect colonies of particles and bioaerosols (Figure 3), so their disposal is an ethical obligation and social responsibility. Therefore, maintenance teams must be aware of the hazardous contamination of the wet and loaded filters (Figure 4) in hospital air-handling units. Furthermore, the build-up of contaminants on the heating/cooling coils compromises the heat transfer mechanism and creates a potential hazard, as shown in Figure 5. Maintenance staff should be better equipped with personal protection to avoid direct exposure to contamination from any segment of the HVAC systems, including porous duct linings, diffusers and drain pans. Adhering to the procedures necessary to minimise exposure to various contaminants underscores the appropriate health and safety issues confronting maintenance teams, which their managers sometimes neglect.
Air quality monitoring
Continuous air quality monitoring devices are the next best incorporations to the facility management toolbox. The devices reveal the physical and chemical characteristics of the air patients, doctors and visitors inhale. They also enable facility management to steer towards data-driven decisions by detecting and responding to air quality deviations from the required standards. The availability and affordability of continuous air quality monitoring systems leaves no excuse for those who oppose the expenditure, as saving a single human life is worth the investment.
Business-savvy facility directors can become co-contributors to air quality enhancements by reinvigorating “fit for purpose” maintenance programmes to accommodate air quality and HVAC demands. Decision-makers in healthcare facilities should focus on providing a sustainable healthy environment, not just cutting filter acquisition and maintenance costs. The stream of paying minimum wages and cutting costs ends in the eerily familiar smudged air diffuser witnessed daily. Chronic and common filter failures accelerate HVAC equipment and hospital ageing faster than planned, leaving the facilities to constantly retrofit and catch up to resolve safety regulations and compliance issues.
Let the sunshine in
Enhancing the healing process in hospital environments requires far more than simple euphemisms about propelling air quality. Instead, authentic engagement involves shared focus and dialogue among urban designers, architects and HVAC filtration experts to avail the integration of technologies to yield sustainable built environments. In addition, advancing air quality considerations to the forefront can shift the hearts, minds and attitudes of decision-makers to make a difference. Initiating healing change from that premise represents learning from the wounds of the pandemic to embarking on a new beginning towards healthy indoor environments. We cannot simultaneously seek cures in hospitals, yet find them contaminated, while decision-makers neglect the danger implicit in the air quality alarms. If providing air quality is a civic right, it must be delivered to eight billion people around the globe, whether they are sick or not. So, as much as we need to open windows to ventilate, we must let the sunshine in and get to the truth about improving hospital air quality.

Figure 1: Different designs to project a pleasant dimension to the hospital environment


Figure 2: Abandoned used air filters in healthcare facilities waiting for appropriate disposal
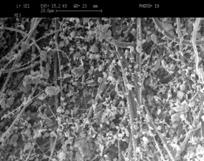
Figure 3: Scanning electron microscopic image illustrating particle-loaded HEPA filter

Figure 4: Wet and loaded filters pose a health hazard in a hospital air-handling unit

Figure 5: Build-up of contaminants on the heating/cooling coils due to inappropriate filtration and leaky installations
References:
[1] J.H. Kwon, K.B. Nickel, K.A. Reske, D. Stwalley, E.R. Dubberke, P.G. Lyons, A. Michelson, K. McMullen, J.M. Sahrmann, S. Gandra, M.A. Olsen, J.P. Burnham, Risk factors for hospital-acquired infection during the SARS-CoV-2 pandemic, Journal of Hospital Infection, Volume 133, 2023, Pages 8-14, ISSN 0195-6701.
[2] Xiaoming Gao, Zakiah Mat Jali, A.R. Abdul Aziz, Hanee F. Hizaddin, Archina Buthiyappan, Jegalakshimi Jewaratnam, Mustapha M. Bello, Inherent health-oriented design for preventing sick building syndrome during planning stage, Journal of Building Engineering, Volume 44, 2021, 103285, ISSN 2352-7102.
[3] J.A. Otter, J. Zhou, J.R. Price, L. Reeves, N. Zhu, P. Randell, S. Sriskandan, W.S. Barclay, A.H. Holmes, SARS-CoV-2 surface and air contamination in an acute healthcare setting during the first and second pandemic waves, Journal of Hospital Infection, Volume 132, 2023, Pages 36-45, ISSN 0195-6701.
[4] Walch JM, Rabin BS, Day R, Williams JN, Choi K, Kang JD. The effect of sunlight on postoperative analgesic medication use: a prospective study of patients undergoing spinal surgery. Psychosom Med. 2005 Jan-Feb;67(1):156-63. doi: 10.1097/01.psy.0000149258.42508.70. PMID: 15673638.
[5] Brzeszczyńska J, Brzeszczyński F. Benefit of sunlight and melatonin on back pain and inflammation. Bone Joint Res. 2023 Mar 7;12(3):199-201. doi: 10.1302/2046-3758.123.BJR-2023-0026. PMID: 37051814; PMCID: PMC10032241.
[6] Bennett NT, Schultz GS. Growth factors and wound healing: Part II. Role in normal and chronic wound healing. Am J Surg 1993; 166: 74–81.
[7] K.I. Quintyne, C. Kelly, A. Sheridan, P. Kenny, M. O’Dwyer, COVID-19 transport restrictions in Ireland: impact on air quality and respiratory hospital admissions, Public Health, Volume 198, 2021, Pages 156-160, ISSN 0033-3506.
[8] Piotr Uścinowicz, Anna Bogdan, Mirosław Szyłak-Szydłowski, Magdalena Młynarczyk, Dominika Ćwiklińska, Subjective assessment of indoor air quality and thermal environment in patient rooms: A survey study of Polish hospitals, Building and Environment, Volume 228, 2023, 109840, ISSN 0360-1323.
[9] Sandra Cabo Verde, Susana Marta Almeida, João Matos, Duarte Guerreiro, Marcia Meneses, Tiago Faria, Daniel Botelho, Mateus Santos, Carla Viegas, Microbiological assessment of indoor air quality at different hospital sites, Research in Microbiology, Volume 166, Issue 7, 2015, Pages 557-563, ISSN 0923-2508.
[10] Tellier, R., 2009. Aerosol transmission of influenza A virus: a review of new studies. J. R. Soc. Interface 6 (Suppl. l_6), S783–S790.
[11] Waqas Khalid, Sheikh Ahmad Zaki, Hom Bahadur Rijal, Fitri Yakub, Investigation of comfort temperature and thermal adaptation for patients and visitors in Malaysian hospitals, Energy and Buildings, Volume 183, 2019, Pages 484-499, ISSN 0378-7788.
[12] A. Nevalainen, M. Taubel and A. Hyvärinen J.S. Pastuszka (Ed.), Synergic Influence of Gaseous, Particulate, and Biological Pollutants on Human Health, Taylor & Francis Group (2015), pp. 176-184.
[13] DIN 1946-4:2018-09 Ventilation and Air Conditioning – Part 4: Ventilation in Buildings and Rooms of Health Care.
[14] Ulrikka Nygaard, Ulla Birgitte Hartling, Jens Nielsen, Lasse Skafte Vestergaard, Kia Hee Schultz Dungu, Jeppe Sylvest Angaard Nielsen, Anna Sellmer, Astrid Thaarup Matthesen, Kim Kristensen, Mette Holm, Hospital admissions and need for mechanical ventilation in children with respiratory syncytial virus before and during the COVID-19 pandemic: a Danish nationwide cohort study. The Lancet Child & Adolescent Health, Volume 7, Issue 3, 2023, Pages 171-179, ISSN 2352-4642.
[15] Ahmad Hassan, Muhammad Zeeshan, Microbiological indoor air quality of hospital buildings with different ventilation systems, cleaning frequencies and occupancy levels, Atmospheric Pollution Research, Volume 13, Issue 4, 2022, 101382, ISSN 1309-1042.
Dr Iyad Al-Attar, an independent air filtration consultant, writes on specific science and technology issues relating to Indoor Air Quality, including airborne particles. He may be reached at iyadalattar@yahoo.com.
Copyright © 2006-2025 - CPI Industry. All rights reserved.